How is Artificial Intelligence being used in the Medical field?
Artificial intelligence (AI) is now a key player in medical research. Its applications range from patient diagnosis and drug discovery to enhancing communication between doctors and patients, interpreting medical records, and providing remote patient care.
What is Artificial Intelligence (AI) in healthcare?
AI in healthcare refers to using machine-learning algorithms and software to replicate human thought processes in analyzing, presenting, and interpreting complex medical data. Essentially, AI involves the ability of computer algorithms to draw conclusions based solely on the input data they receive.
The primary goal of AI applications in healthcare is to explore connections between clinical practices and patient outcomes. AI programs facilitate various activities, including diagnostics, treatment protocol development, drug discovery, personalized medicine, and patient monitoring. What sets AI apart from traditional healthcare technologies is its ability to gather and process data, ultimately producing clear outcomes for users. AI achieves this via machine learning algorithms and deep learning techniques, which can identify patterns in behavior and develop their own reasoning.
For AI models to yield useful insights and predictions, they must be trained on large datasets. AI algorithms operate differently than humans in two primary ways:
- Algorithms are factual: once a goal is established, the algorithm learns exclusively from the input data and can only execute what it has been programmed to do.
- Some deep learning algorithms are black boxes; they can make highly accurate predictions but offer little understandable reasoning behind their decisions aside from the data and type of algorithm used.
How is Artificial Intelligence (AI) being used in the Medical Field?
- AI supports clinical imaging analysis:
AI serves as a triage tool for clinicians, assisting them in reviewing images and scans. This technology helps radiologists and cardiologists spot critical insights that enable them to prioritize urgent cases, avoid potential misinterpretations of electronic health records (EHRs), and make more accurate diagnoses.
A clinical report often generates vast amounts of data and images that need to be analyzed. AI algorithms can quickly process these datasets, comparing them with past studies to identify patterns and remote connections. This capability allows imaging professionals to extract essential information swiftly.
- AI has the potential to reduce the cost of drug development:
Supercomputers are leveraged to predict molecular patterns where potential drugs may not be effective against various diseases. Utilizing convolutional neural networks, technology like AtomNet has been able to forecast how small molecules bind to proteins by analyzing vast amounts of experimental data and protein structures. This method enables the identification of safe and effective drug candidates from extensive datasets, ultimately lowering drug development costs.
- Unstructured data is analyzed by AI:
Healthcare professionals often struggle to keep current with the latest clinical advancements while providing high-quality, patient-centered care due to the overwhelming amount of health data and records. AI can rapidly sift through EHRs and biomedical information from clinical units, delivering timely and accurate responses to clinicians.
Much of the health data and patient records are stored in complex, unstructured formats, making them difficult to navigate and interpret.
Rather than being overwhelmed by the need to search for, identify, compile, and transcribe critical information, AI can efficiently seek, gather, store, and standardize medical data in any format. This innovation helps streamline routine tasks and equips healthcare providers with quick, effective, and tailored treatment options for patients.
- AI creates complex and integrated drug discovery platforms:
AI algorithms can uncover new drug applications, assessing both their safety profiles and mechanisms of action. This technology has led to the development of clinical research platforms that enable the repurposing of existing drugs and explore their bioactivities.
By merging the best aspects of biology, data science, and automation with advanced AI technologies, the foundational company of this platform can process around 80 terabytes of biological data weekly across 1.5 million studies.
- Artificial Intelligence can help diagnose kidney disease:
Acute kidney injury (AKI) can be challenging for clinicians to detect, yet it can lead to rapid patient deterioration and mortality. With an estimated 11% of hospital deaths attributed to failure in identifying and treating AKI patients, early prediction and intervention can significantly reduce the overall need for long-term treatments, including kidney dialysis.
- AI serves as a valuable resource for emergency health workers:
In the event of a heart attack, the time from emergency call to ambulance arrival is critical for patient survival. For greater chances of recovery, emergency dispatchers must quickly recognize heart attack symptoms. AI can analyze both verbal and nonverbal cues to facilitate accurate diagnoses during these critical moments.
Corti is an AI tool designed to aid emergency medical personnel. It analyzes the caller’s voice, background noise, and relevant patient data to alert emergency responders of a potential heart attack. Similar to other machine learning technologies, Corti does not search for specific symptoms but instead trains itself to recognize urgent indicators by processing a vast range of information.
Future of Artificial Intelligence (AI) in healthcare 2023?
As we move forward, AI is poised to add value by either automating or enhancing the roles of clinicians and staff. Many repetitive tasks will become fully automated, and AI can serve as a valuable tool that helps healthcare professionals excel in their work, ultimately improving patient outcomes.
With its ability to streamline processes, AI has the potential to enhance both the quality of life for clinicians and patient experiences in hospitals and medical practices nationwide. As we step into 2023, healthcare providers can increasingly leverage AI to optimize the care process.
Voice recognition technology is increasingly taking the place of traditional dictation in various healthcare information systems, including Electronic Health Records (EHRs). Not only can voice recognition significantly cut down transcription costs, but it also has the potential to reduce transcription errors. But does it outperform humans when it comes to understanding and interpreting spoken words? For the most part, the answer is yes, particularly when the system is properly “trained.” Generally, a physician can begin using voice recognition and expect an accuracy rate of around 95%.
The way voice recognition technology processes spoken language allows it to convert words into specific data entries, rather than just creating unstructured text blocks. When an EHR system is effectively designed to support dynamic, command-based interactions, the voice recognition feature becomes highly intuitive. For optimal use, physicians should avoid speaking in full sentences or providing extensive narratives. An EHR can be programmed to respond dynamically to specific procedures, techniques, symptoms, and care plans. By incorporating thousands of these command-based responses, an EHR system can greatly reduce the time it takes to perform conventional dictation. Additionally, physicians can train the system with their own voice, making adjustments in real-time to the text within the EHR, which can be stored in the cloud. This allows them to access their voice files and document information during patient visits, whether onsite or on the go.
EHR information serves multiple functions. It is crucial for compiling a thorough medical history, supporting clinical research, and ensuring accurate diagnoses and treatments. While handwritten notes are becoming less common, some physicians still prefer this method due to familiarity. Traditional dictation and transcription require significant labor, leading to a dwindling number of skilled medical transcriptionists as more practices transition to digital record-keeping. The U.S. Bureau of Labor Statistics predicts a slight but steady decline in available jobs for medical transcriptionists over the next decade. Moreover, trained voice recognition can alleviate many concerns about EHR systems that are often viewed unfavorably. Without voice recognition, physicians often face a cumbersome series of screens, tabs, and checkboxes, resulting in 5 to 12 minutes spent on 100 mouse clicks and extensive manual data entry just to document a single exam note. This has left many physicians feeling frustrated as they struggle to find enough time for patient interactions, often resorting to data entry after hours. In contrast, with trained voice recognition and dynamic command-based responses, a simple exam note could take only 90 seconds to complete, helping to mitigate physician burnout.
By integrating an EHR system with trained voice recognition, a medical practice can save valuable time and money, ultimately allowing physicians to see more patients.
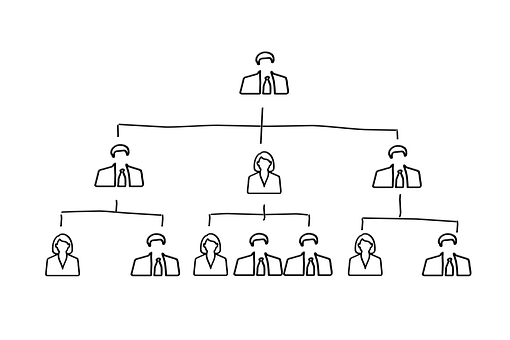
What is a Hierarchy in Healthcare?
Most healthcare organizations today, including the National Health Service (NHS), operate under a hierarchical, pyramidal leadership model. This type of leadership is characterized by a “clearly defined chain of command that extends from the lower to the upper levels of an organization.”
Structure of Hierarchy in Healthcare
Typically, larger organizations possess a hierarchical structure based on various levels of authority, forming a chain of command that interlinks multiple management tiers within the organization. Decisions are usually made in a formal, top-down manner.
What is the Hospital Hierarchy?
The hierarchy within hospitals can differ by location, but it generally features a general manager and medical directors at the top, with medical assistants at the bottom.
Here’s an overview of the typical hospital hierarchy, starting from senior positions to lower-level roles:
- Manager in Charge:
This top-level official oversees the hospital’s administration, responsible for crafting and implementing policies that ensure patient safety and promote recovery. They also manage the hospital’s financial health regarding budgets and the operational viability of different departments.
- Medical Executives:
Larger hospitals often have multiple medical directors, while smaller ones might only have one or two. These directors are tasked with formulating safe and effective healthcare policies and should always be aiming to uphold high standards of patient care. They oversee nearly all aspects of both inpatient and outpatient services, with some managing specific teams of specialists while others provide more general oversight. Every physician in the hospital reports to a medical director.
- Department Head:
Department heads are specialized doctors leading fields such as orthopaedics, oncology, and pediatrics. In a hospital setting, they create and coordinate medical strategies, guiding attending physicians who follow their direction. Should an attending physician be unavailable due to emergencies, department heads may step in to assist.
- Attending Physician:
Attending physicians are senior doctors responsible for overseeing patient treatment plans. They must possess a minimum of three years of residency experience, with many working in specialized areas.
- Nurse Practitioner:
Nurse practitioners typically interact with patients directly, providing urgent, primary, and specialized care to specific populations, including children, women, and the elderly. Their duties include documenting medical histories, collecting patient samples, ordering lab tests, and performing a variety of direct patient care tasks.
- Pharmacist in a Hospital:
Pharmacists dispense prescription medications and guide patients in their safe use. They may also conduct health screenings, administer vaccines, and oversee medication management in the hospital.
- Specialist in Clinical Nursing:
Clinical nurse specialists can order tests, make diagnoses, provide basic treatments, and in certain states, prescribe medications within a hospital. They also offer expertise and support to the nursing staff.
- Nurse Technician:
Nurse technicians receive additional medical training beyond standard nursing, allowing them to undertake more technical tasks such as inserting catheters, removing stitches, and operating advanced monitoring equipment.
- Registered Nurse:
In a hospital, registered nurses (RNs) handle a broad array of responsibilities, including prepping patients for exams and treatments, administering medications, and educating patients and their families about care processes.
- Assisting in the Medical Field:
Medical assistants represent one of the entry-level positions in hospitals, engaged in various administrative tasks. They may schedule patient appointments, follow up on care, and assist with bookkeeping and billing, most of their work taking place at a desk.
Why is Hierarchy Beneficial in Healthcare?
The fundamental purpose of hierarchy is to help us navigate the complexities of the world, simplify information, and facilitate decision-making. Think of it evolutionarily: when someone declared, “Throw the spear now to take down the mammoth,” their leadership was vital.
A well-established hierarchy holds leaders accountable for outcomes and sets up mechanisms for replacing ineffective leaders, sometimes through promotions from within. This structure ultimately contributes to the success of the organization as a whole, encompassing owners, managers, and employees alike.
What is the Purpose of Hierarchy in Healthcare?
As employees ascend the hierarchical structure, their level of authority increases. Authority is essential whenever leadership is necessary, ensuring that those under a manager work collectively towards the organizational goals—or face potential consequences.
Every day, online retailers guide us through various step-by-step processes—whether it’s buying a pair of jeans, applying for a MasterCard, or booking a flight—using digital transactions. These electronic paths ensure that we rarely make mistakes; if we miss an essential piece of information or choose incorrectly, the system won’t let us continue until we correct it. In systems engineering terms, this process is referred to as “mistake-proofing.” In the rare case that we encounter a complex or unfamiliar transaction, we might end up calling for help from a knowledgeable expert. This concept of mistake-proofing translates well to electronic medical records (EMR), which can lead us towards safer, higher-quality, and more affordable healthcare.
EMRs enhance patient safety by using computer-based physician orders that eliminate issues caused by unreadable handwriting and misunderstood verbal instructions. Features like checkboxes ensure only the correct medication doses are available, reducing the risk of overdoses. Nurses now verify that the right patient receives the appropriate treatment by matching a code on the patient’s wristband with the medication label; these crucial safety features are seamlessly integrated into everyday practices via the EMR. Furthermore, the EMR acts as a foundation for innovation and creativity, as it provides structured prompts to both standardize and enhance patient care.
From our experience, three fundamental factors stand out. First, it is essential to establish best-practice standards that minimize unnecessary variation in managing medical conditions. Healthcare groups implement these measures with a shared commitment to quality, and medical science societies play a role, even though they lack the authority to enforce standards. They can, however, help foster alignment on broadly accepted recommendations across U.S. medical practices. For example, the Choosing Wisely initiative, launched in 2012 by the American Board of Medicine in collaboration with Consumer Reports, involves 70 professional societies offering recommendations intended to engage providers and patients in meaningful discussions to avoid unnecessary treatments.
Second, it’s crucial for medical centers and vendors to collaborate in integrating more protocols into EMRs that aid physicians in making straightforward decisions. A focal point should be the development of “hard stop” tools—mechanisms that prevent unsafe or inappropriate care (like ordering unnecessary imaging tests). While some of these EMR applications are in initial stages of development, one significant challenge is the cost associated with dedicating clinical and technical staff to implement and maintain these projects. As medical centers face increasing financial pressures, the expense can hinder the custom development of such tools.
Providers who fully utilize the capabilities of the EMR stand to benefit from increased market share and reduced costs. Most importantly, it enables doctors to leverage the powerful protection of digital mistake-proofing along with their expertise in providing care to their patients.
In today’s healthcare landscape, artificial intelligence is becoming increasingly prevalent, leading to transformative digital advancements. As new tools and resources emerge, many developed nations are actively adopting AI-driven technologies, particularly voice-activated and digital assistants, marking a significant shift from a physician-centered approach to a model that prioritizes patients.
Electronic Health Records (EHR) play a crucial role in converting patient information from physical files to digital formats. While EHRs have done an admirable job of securely collecting and storing patient data, they have evolved beyond just record-keeping in recent years.
In medical facilities worldwide, information technology has become essential for healthcare providers. EHRs have transitioned from simple storage solutions to comprehensive systems that facilitate data sharing among physicians, patients, and specialists. Some software offers valuable insights that support clinical decision-making by giving healthcare professionals a broader understanding of patient histories and treatment options. Overall, EHRs are positively impacting public health outcomes across the globe.
Most healthcare providers recognize that electronic data systems enhance patient care, while some also appreciate the clinical benefits these tools bring to their practices. Many medical institutions are exploring technological advancements such as data standardization, artificial intelligence, and predictive analytics to optimize EHR systems and refocus their efforts on improving patient care.
How EHRs Enhance Patient Care:
Electronic health records, once viewed merely as data entry systems, are now placing patients at the center of their care. These digital solutions boast advanced features that facilitate the analysis of patient information, enable communication among healthcare professionals, and allow for secure information sharing. Today’s EHR systems provide essential tools that help streamline operations and enhance patient outcomes. Below are some key ways EHRs have demonstrated their ability to improve patient care over time.
Improved Patient Engagement
EHR software is vital in closing the gap between patients and providers. Its integrated features assist clinics in daily operations while enhancing patient satisfaction. When visits overwhelm patients with information, they may not fully grasp what is shared. However, through patient portals, they can access important documents at their convenience. Additionally, the ability to send online prescriptions directly to their preferred pharmacies boosts patient satisfaction and adherence. When patients feel informed about their health journey, they’re more likely to follow their provider’s recommendations. Keeping them engaged throughout the process fosters compliance and a smoother experience.
Focus on Preventive Care
Electronic medical records offer robust management tools that help monitor various health conditions. They assist healthcare providers in reminding patients about check-ups and screenings. EHR systems can also identify risk factors and health habits, enhancing preventive care strategies. By receiving timely reminders for essential screenings, patients can better educate themselves and address potential health risks. Early detection of health issues can be life-saving and can help prevent complications.
Better Patient Outcomes
Clinic-based EHR systems enable administrative staff to collect, record, store, and monitor patient health information seamlessly. Healthcare providers, including doctors, nurses, and lab technicians, gain a comprehensive view of patient interactions, leading to improved outcomes. EHRs centralize patient data, allowing for the identification of health trends and better analytics that support decision-making. This results in more effective treatment plans and ultimately enhances the quality of clinical care patients receive.
Final Words
The transition from traditional medical record systems to EHRs has a significant impact on the quality of patient care delivered. With the help of SimboAI, the future of healthcare is here! From intelligent robots to e-prescriptions, SimboAI is revolutionizing the landscape of Medicare.
Top 5 Healthcare Hazards for 2023
Healthcare encompasses the improvement of health through the prevention, diagnosis, treatment, and management of diseases, injuries, and various physical and mental disabilities.
In 2023, there will be a stronger emphasis on primary care, widespread availability of telemedicine, and the integration of AI to improve patient outcomes. Healthcare professionals will also be exploring methods to cut costs while enhancing patient satisfaction and overall experience.
Current Challenges Facing Hospitals:
The healthcare landscape is diverse, with advanced technologies, skilled professionals, and well-equipped facilities on one side, while on the other, we face the challenges of an aging population and escalating healthcare costs. Both sides are striving to adapt to the uncertainties that lie ahead.
Below are some of the challenges that hospitals are currently encountering:
- Rising Medical Costs:
The healthcare cost crisis is not new. Various stakeholders—including payers, medical device manufacturers, and health plan providers—impact the pricing of healthcare services.
With so many parties involved, conflict is inevitable. Reaching an agreement requires careful planning and patience.
These rising costs directly affect healthcare organizations’ revenue, as patients may hesitate to go for routine follow-ups or lab tests due to financial concerns, ultimately leading to poorer clinical outcomes.
- Financial Strain and Hospital Productivity:
With healthcare costs climbing globally, hospitals are the second-most energy-intensive establishments after restaurants. Combined with an aging population and increased energy prices, these financial strains pressure institutions to provide better care with fewer resources.
- Ensuring Patient Safety:
An estimated 20,000 Americans and 5,000 immigrants die each year from infections acquired during medical treatment. Reducing the risk of infections, along with other threats like power outages, is crucial for delivering high-quality patient care and maintaining the organization’s reputation.
- Regulatory Compliance and Energy Standards:
Failing to adhere to regulations can disrupt operations, lead to inadequate care, create safety issues, and result in significant penalties. Many countries are pushing health clinics to cut their carbon footprints and meet energy reduction mandates as demand for energy rises.
- Hospital Security:
Healthcare facilities are often open around the clock, putting visitors under significant stress during critical times. Issues such as drug theft, vandalism, child abductions, and wandering patients represent serious security challenges.
- Patient Satisfaction:
Effective treatment impacts both the length of hospital stays and the likelihood of rehospitalization. The American Society for Healthcare Engineering (ASHE) notes that patients are generally discharged from high-quality hospitals about 2.5 days earlier than from traditional ones. Patient satisfaction also affects hospital revenue; quality metrics may decline if systems fail to operate effectively.
Top 5 Hazards in 2023:
The following list reflects the collective assessment of the health technology hazards that should be prioritized in 2023. While many previously identified risks remain significant—including the need for robust cybersecurity measures, noted as the top threat in 2022—there are new challenges that require immediate attention.
The ECRI (Emergency Care Research Institute) report highlights several industry challenges for 2023, urging manufacturers to develop processes or devices that reduce or eliminate these risks. Given the staffing shortages and high stress among healthcare employees, it is vital to innovate technologies that ensure safe use.
- Medication Errors from Improper Use of Automated Dispensing Cabinets:
Automated Dispensing Cabinets (ADCs) are designed to provide controlled access to medications near the point of care. However, these cabinets often contain locked drawers or compartments for drug storage. Healthcare professionals must ensure that the medications they provide, verified by a pharmacist, are used correctly to avoid errors.
- Potential Care Disruptions from Cybersecurity Threats to Cloud-Based Systems:
While using cloud technology for clinical services like electronic health records (EHR) offers numerous benefits over traditional systems, it also introduces security risks that cannot be ignored. Organizations that overlook these risks may face severe security breaches that compromise healthcare quality and put patient information at risk.
- Patient Risks from Gaps in Communication About At-Home Medical Devices:
Patients using home medical devices often lack clear and accurate information regarding issues or recalls, leading to a growing awareness gap as care increasingly shifts to home settings.
- Risks Associated with Forgotten Arterial Needles:
Hemodialysis carries significant risks, especially if a central venous line becomes disconnected or the venous needle detaches. Such events can lead to rapid blood loss or severe injury, often without adequate alarm signals from the hemodialysis machinery.
- Ongoing Risks Due to Reporting Gaps Related to Device Issues:
Reporting problems with medical devices is crucial for ensuring safety among healthcare staff and patients. Unfortunately, many issues go unreported, and healthcare organizations need to identify and eliminate barriers to accurate reporting. Streamlining the reporting process is essential to minimize disruptions in patient care and enhance safety by fostering an environment conducive to reporting, training staff to recognize risks, providing timely feedback, and celebrating successes where reports have prevented harm.
Ways to Mitigate Healthcare Hazards:
By understanding the risks associated with various hazards, we can take proactive measures to reduce or eliminate them.
- Eliminate the hazard altogether.
- Substitute the hazard with a less risky alternative.
- Isolate the hazard.
- Implement administrative controls.
- Follow standard precautions.
- Use personal protective equipment.